Vaccinating vulnerable populations
“People were stuck, bed-ridden or homebound and wanted to be vaccinated”

While thousands of Australians were lining up at vaccination centres or visiting their GP or chemist to receive a vaccination to protect themselves from COVID-19, many were left stuck at home and unable to make the journey to receive the same privilege.
Ironically, many of those homebound were older people, or suffered from a medical condition – increasing their risk of adverse effects should they be unlucky enough to catch COVID-19.
One North Brisbane resident had been trying for months to get a vaccination for her mother, who had significant mobility issues which left her homebound. Anxious that her mother would contract COVID from one of the care staff coming to her house regularly, she contacted a long list of health professionals and even politicians to find someone who could help.
She contacted Dr Deborah Mills who runs the clinic Dr Deb The Travel Doctor in Brisbane CBD.
“People were desperate for the vaccine,” said Dr Mills “We got calls because people thought we were a ‘travelling’ clinic. Homebound persons were stuck bed-ridden but they still needed to be vaccinated.” Our clinic had no travellers to vaccinate, so we had the time to do this.
Dr Deb and her team were able to administer the vaccine to this particular resident’s mother in their lounge room.
“The daughter was incredibly relieved and pleased that her mother was able to be better protected from COVID-19.”
Dr Deb and her staff conducted many home visits to vaccinate people who could not leave their homes: one doctor, one nurse, and a pile of gear travelled around the north Brisbane suburbs, —usually it took well over one hour to vaccinate one person.
“Each person we saw was different, and each person had a story. One man was a paraplegic. Someone else was housebound because of a psychiatric illness.
“There was one patient with fragile mental illness who had gone to the chemist for his first dose, but being vaccinated was too overwhelming an experience for him and he had a severe panic attack so he had not been able to get any subsequent doses. “Our team is very familiar with giving immunisations and helped him feel comfortable, plus he was at home so he managed his second dose with flying colours”.
“Another person was stuck in a wheelchair in his house. He had minimal support as his family were in Melbourne. Without someone coming to his house he just couldn’t get vaccinated.”
Brisbane North and Brisbane South PHNs funded Micah Projects and QuIHN to also make COVID-19 vaccines available to people who were unable to book and present to regular vaccination outlets.
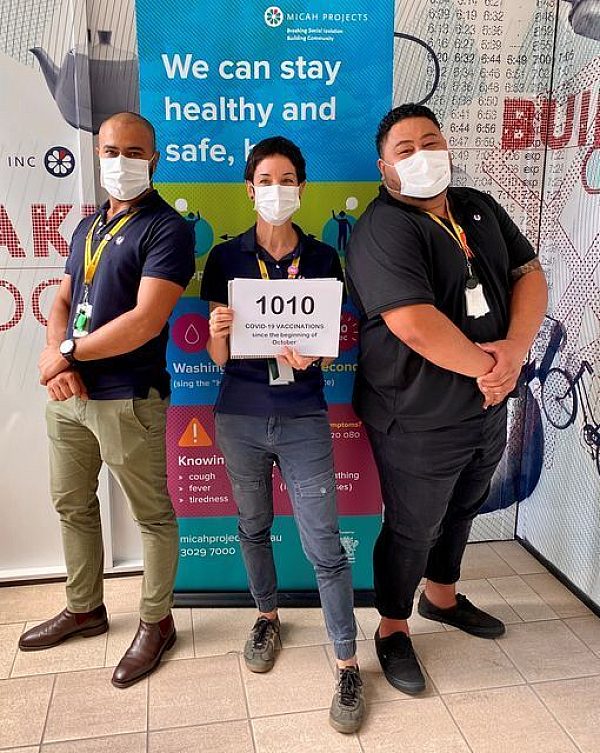
From the end of September through to December 2021, Micah’s pop-up clinics and Inclusive Health Clinic administered 1010 vaccinations to a broad demographic of vulnerable people.
Micah staff knocked on over 1,800 doors to offer vaccines and transported more than 170 people to vaccination sites. A total of 56 pop-up clinics were conducted across the Brisbane region including Brisbane North.
Dr Mills also received a call from Micah Projects to help vaccinate the homeless in our community.
“One afternoon, we set up on the porch of a boarding house in Spring Hill. We checked the Australian Immunsation Register from our laptops. When darkness fell, the porchlight was broken, so we pulled out torches and I thought: ‘This must be happening all over the world, medical staff vaccinating people in difficult circumstances.”
These services also came with significant learnings, including how to ensure the vaccination certificate reached the individual. Many individuals assisted by the Micah Program don’t have phones or easy access to service providers, staff often sat with them for hours helping to link and access information.
“Many do not know the last GP they went to, what bank account is associated with Medicare, or other details that are needed in setting up everything online,” one Micah staff member said.
“The sense of urgency wrapped in the lack of resources, health, and accessibility is a daunting and tedious process for vulnerable population groups.”
Dr Mills also said working through administration was a challenge. “Some people had no Medicare card, some had two names, someone else had two Medicare numbers linked to the one name – it was quite a challenge to work through all the administrative issues that went with recording the vaccine.”
These outreach services were met with immense gratitude from the community. As one Micah nurse said, “Our clinics have provided a space for those who wouldn’t present to a vaccination hub, hospital, or local GP. By going to the areas they live, we have been able to increase our care and build the trust necessary for their continued well-being.”
Dr Mills said it was a privilege to go out and meet so many lovely people. “People were extremely happy to protect their loved ones and being able to do so really lessened their anxiety around COVID.”
Where people who are housebound and are having difficulty accessing a vaccination, they, their service provider, carer or family can contact the PHN for support in finding a provider, or to arrange an in-home vaccination. Find out more.
