
Announced: North Brisbane and Moreton Bay Medicare Mental Health Centres opening from July
Mar 27, 2025
Mar 15, 2021
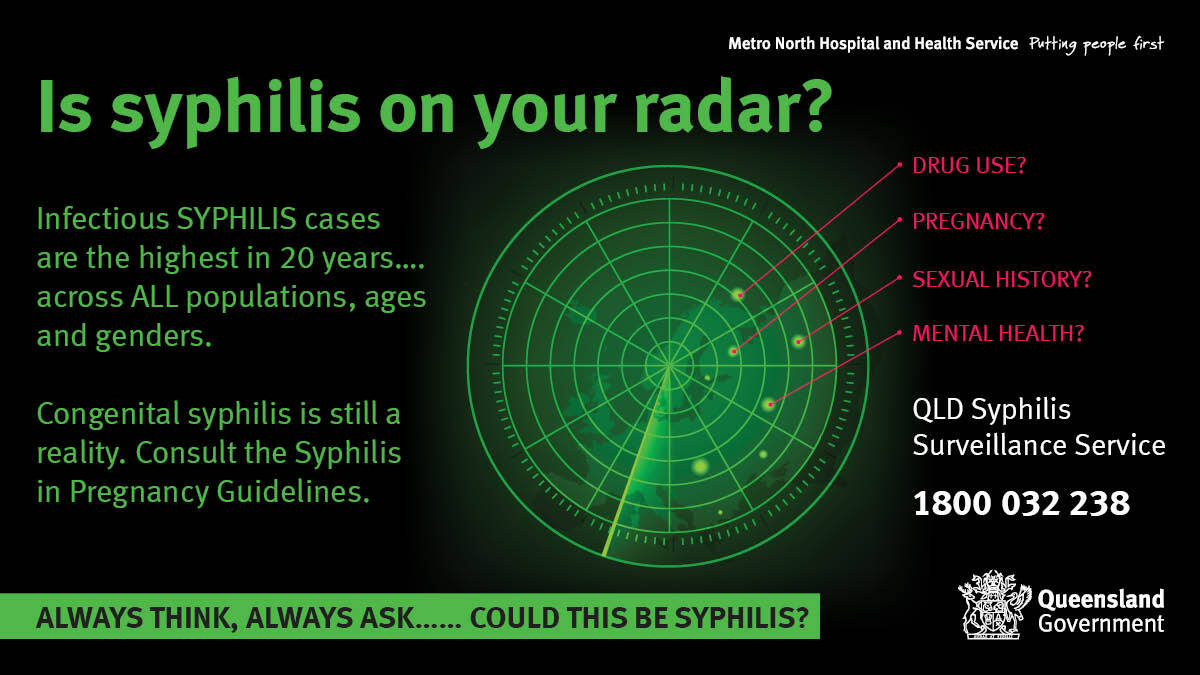
In the previous five years, a series of emerging syphilis outbreaks have been observed across South East Queensland, transitioning from a predominantly men who have sex with men (MSM) focussed infection to one affecting heterosexual men, women and transgender persons.
The numbers of notifications for southern Queensland have now increased by 100 per cent since 2016. The proportion of female cases has increased fourfold from 2015 to 2020. Correspondingly, the proportion of notifications reported amongst MSM has decreased while numbers of heterosexual men have doubled in the last 3 years. An increasing proportion of notifications are being diagnosed through general practice, accounting for almost half of all notifications in 2020.
The implications for antenatal transmission and congenital infection are significant and serious.
Clinical presentations of syphilis can be diverse, and many infections are asymptomatic but transmissible. Many health care providers will have challenges with the lack of familiarity with syphilis.
Limitations on time, expertise and resources to deal with the complexity that can arise with such cases may lead to delayed diagnosis and sub-optimal management of infection, particularly amongst women. Even when correctly diagnosed, issues of correct treatment and essential partner notification can become problematic, resulting in potential loss to follow-up and failure to stop further transmission of infection, including the potential for antenatal and congenital infection.
Healthcare providers should be alert to the possibility of syphilis in their patients, particularly those who may present with a history of alcohol and/other drug or mental health issues, housing instability, economic stress or social marginalisation.
GPs should be particularly attentive to their antenatal patients. This requires awareness of the latest clinical guidelines, awareness of the range of symptoms that may suggest primary or secondary syphilis, and awareness of potential risk indicators in a patient’s history. Syphilis should not be considered in isolation, but within the context of a broader sexual health check or blood borne virus screen. A test for Hepatitis C, Hepatitis B,
or HIV should routinely include syphilis serology and the opportunity for further STI testing.
Any concerns with a syphilis presentation can be discussed with the Queensland Syphilis Surveillance Service (QSSS) and an expert practitioner. The QSSS is a state-wide database containing serology and treatment history of people who have previously had positive syphilis serology.
Healthcare providers who require assistance for patients with positive syphilis serology can contact the QSSS on 1800 032 238.
To access the Syphilis in pregnancy guidelines visit the Queensland Health website.

We acknowledge the Traditional Custodians within our region: the Jagera, Turrbal, Gubbi Gubbi, Waka Waka and the Ningy Ningy peoples of where we meet, work and learn. Brisbane North PHN is committed to reconciliation. Our vision for reconciliation is where the stories of our First Nations’ people are heard and shared, and networks are formed.